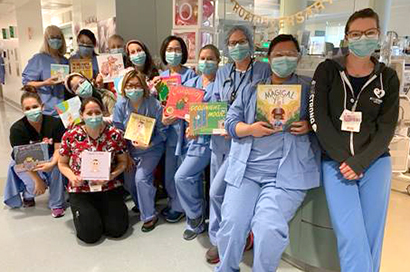
- Rebekah Babcock, RN
- Dana Baicher, RN
- Losana Blair, RN
- Anna Celestino, RN
- Jody Charles, RN
- Cathy Chin, RN
- Laura Haselden, RN
- Annie Le, RN
- Tammy Lee, RN
- Merry Ann Loukianoff, RN
- Michele Lucido, RN
- Terri Muench, RN
- Julie Plank, RN
- Michelle Wrench, RN
ROAR in the NICU
The Family Centered Care Team of the Mountain View Neonatal Intensive Care Unit (NICU) focuses on improving patient outcomes by introducing evidence-based practices and conducting research in the department. One of the new practices the team brought to the NICU is the Reach Out and Read (ROAR) program. Evidence demonstrates that reading to NICU babies helps with bonding and with soothing the infant, even when the parent cannot hold them.
The team created bags with a special logo, filled with books, and distributed 111 of them to NICU families. The time parents spent reading to their babies was measured throughout 2020, and increased significantly to 26 minutes per day by December 2020.
