Protecting Our Most Vulnerable Patients
The Progressive Care Unit (PCU) houses some of El Camino Health's most vulnerable and complex patients. The PCU staff are challenged daily with ethical dilemmas, difficulties with patient flow, and high-risk patients. Despite these obstacles, the PCU staff has prioritized patient safety and improving qualities outcomes. Areas of focus include:
| |
Fall ReductionOne of the PCU's biggest challenges during FY22 was the issue of patient falls. To address this need, daily fall prevention audits were implemented in the department. Our staff on the day shift and night shift assessed the fall risk for each patient and ensured fall prevention interventions were in place. These interventions include:
These audits began in June 2022, the start of FY2023, and to date the department had only one fall, which is a 60% reduction in falls for the department. The PCU also achieve the milestone of being fall-free for more than 120 days. | 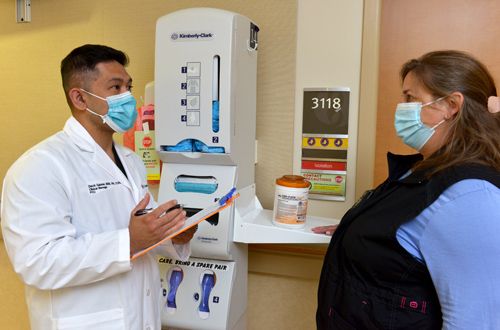 Best Practices in Infection Prevention: |
Reducing C. DifficileHospital acquired infections (HAI) have been a large area of focus for El Camino Health. One of the biggest challenges for our frontline staff is reducing the spread of C. difficile, and the PCU HAI committee representatives have taken extra steps to reducing C. difficile. Brenda Gaidies-Smith, RN and Angela Gates, RN initiated a "C. diff audit form," a tool that the charge and resource nurses use to ensure that all appropriate C. difficile interventions are in place, which include:
We also used surgical caps to cover the alcohol dispensers in patient rooms, which encouraged everyone to wash their hands with soap and water. The audits we had in place along with promoting proper hand hygiene resulted in no hospital acquired C. difficile cases in more than 90 days. The PCU team has demonstrated that going back to the basics of nursing care, practicing nursing diligently, and reinforcing best practices can result in outstanding patient outcomes and improve quality of patient care. The team will continue to reinforce these practices until we achieve our enterprise goal of Zero Preventative Harm. | |
Fall Prevention
Fall injuries have significant implications on disease trajectory and outcomes on cancer patients. Approximately one in 10 falls result in injuries, such as hip fracture, subdural hematoma, and traumatic brain injury. Older patients with cancer and chemotherapy toxicity have additional risk factors for falls. In 2019, the 32-bed inpatient medical-surgical oncology unit had 19 fall incidents. Care team members explored interventions to improve fall prevention and reduce the number of falls. | |
 Fall Prevention: Keeping Our Patients Safe | Our team utilized apparent cause analysis (ACA) and root cause analysis (RCA) to extensively review our falls incidents. We explored the "Five Why's" to identify improvement opportunities and best practice interventions. Interventions to improve falls included:
|
Our direct care staff leading fall prevention initiatives continue to share our lessons learned with the entire team to increase awareness and risk assessment proficiency. This led to a reduction in falls from 2021 to 2022. ACA and RCA revealed common causes, which our team maximized to keep our patients safe. | |
Enhanced Recovery after Cesarean (ERAC) Interdisciplinary Committee
Increases in patient census and acuity within Maternal Child Health (MCH) has led to capacity and staffing concerns. The average length of stay for patients having scheduled cesarean birth at term was 3.27 days with 21.6% of these patients being discharged home on post-operative day four. The Enhanced Recovery After Cesarean (ERAC) Committee was formed in October 2022 with the following goals:
The interdisciplinary committee consists of obstetricians, anesthesiologists, direct care nurses, educators, lactation specialties, managers, service line director, clinical nurse specialist, and administrative analysts. Zoom meetings were conducted every two weeks. | |
A consensus statement by the Society of Obstetric Anesthesiologist and Perinatology (SOAP) was published in 2021 aimed to provide evidence-based recommendations along with level of evidence recommendations for patients having cesarean birth. The ERAC improvement committee reviewed and evaluated implementation feasibility of 24 recommendations that occur during the five phases of care of surgical birth:
|  Early Recovering After Cesarean Section: |
Implementation was carried out individually and in small groups. The members reported on progress, addressed barriers, and discussed the interventions they were working on at scheduled meetings. Forty-eight patient interviews were conducted from November-December 2022. Based on audit findings, recommendations were prioritized based on greatest need. For example:
For the past four months, education that included data reports highlighted bimonthly progress at every Labor & Delivery and Mother Baby Partnership Council meeting. Further nursing education was presented at every staff nurse meeting, in emails, at shift huddles at Mountain View and Los Gatos Campuses. In the mother-baby unit, audits are beginning to reflect improvements in Foley catheters being removed as 6-12 hours after surgery. Additionally, our average length of stay has decreased from 3.27 days to 2.59 days with only 8.7% of patients staying four post-op days, down from 47.6%. The ERAC improvement interventions will now be applied to patients with unscheduled surgical birth. The committee will continue to work on full implementation of all recommendations aimed to optimize surgical recovery. | |
