
請點擊此轉換成中文
Psoriasis is a chronic autoimmune skin disease that affects over 60 million adults and children worldwide. Because psoriasis causes visible skin changes, people sometimes wrongly assume it’s contagious. It is not – as an autoimmune condition, psoriasis is absolutely not transmissible.
With psoriasis, the immune system is over-active and produces messenger proteins called cytokines that prompt skin cells to multiply too fast. Instead of the normal 30 days it takes for the cells to grow and shed, they grow and mature in three or four days, pile up on the surface of the skin, and form itchy plaques covered by silvery scales. These plaques can be different sizes and thicknesses. On light skin, they usually appear pink and sometimes red or even purple. On dark skin, the plaques look dark or reddish brown or grey. Psoriasis can also affect the nails, causing pitting, discolorations, breakage, and even separation from the nail bed.
Researchers are still trying to pinpoint what causes the immune system to attack healthy skin cells. Family history is a risk factor for psoriasis, so there does appear to be a genetic aspect to the condition. However, people with no such family history can and do develop psoriasis. Environmental triggers such as a streptococcal infection, chronic stress, smoking, obesity, and alcohol consumption may contribute to the onset of psoriasis. Certain drugs like chloroquine, lithium, beta-blockers, steroids, and NSAIDs can aggravate symptoms. Although the mean age of onset is 33, psoriasis also occurs in children. The condition is equally prevalent among women and men.
Co-occurring Conditions and Complications
Compared to the general population, people living with psoriasis have higher rates of metabolic syndrome, kidney disease, diabetes, heart disease, Crohn’s disease, lymphoma, skin cancer, celiac disease, non-alcoholic fatty liver disease, and joint problems. A form of chronic inflammatory arthritis called psoriatic arthritis affects 30% of patients with psoriasis and involves painful inflammation of the joints and connective tissue commonly affecting the joints, particularly in the fingers and toes. Psoriasis can also occur around and even in the eyes. Not surprisingly, psoriasis takes an emotional toll on patients and makes them more prone to depression, alcoholism, substance abuse, smoking, and suicide.
Types of Psoriasis
The type of and severity of psoriasis a person has can vary over time, and it’s possible to have a flare up of several types at the same time.
- Plaque psoriasis accounts for 80-90% of psoriasis cases. It's characterized by raised patches of inflamed, itchy, painful scaly skin. Lesions can appear anywhere on the body but are most common on the scalp, knees, elbows, belly button and lower back.

- Guttate psoriasis affects roughly 8% of those living with psoriasis. The condition typically emerges in childhood or early adulthood, often triggered by a bacterial infection such as strep. Guttate psoriasis presents as small, round red or discolored spots. It can affect any area of the body.

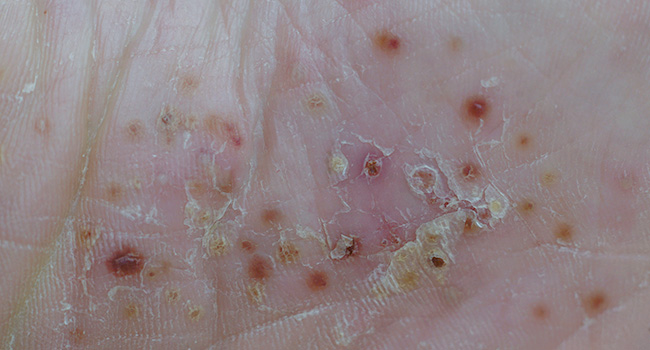
- Pustular psoriasis creates pustules, white, painful pus-filled bumps surrounded by inflamed, red or discolored skin. The condition accounts for 3% of the psoriasis cases. It can appear anywhere on the body but often favors the hands and feet. Pustular psoriasis is a serious condition that can lead to systemic inflammation, organ failure, and sepsis. A flair up requires swift medical attention.
- Inverse psoriasis affects skin folds, such as underarms, genitals, buttocks, and the area beneath the breasts. The skin remains smooth but is inflamed and deep red or darkened. This form of psoriasis can cause severe pain and itching. An estimated 25% of those living with psoriasis have or have had eruptions of inverse psoriasis.
- Erythrodermic psoriasis, which affects roughly 2% of those living with psoriasis, is rare but potentially life-threatening as it can affect the whole body. It causes intense discoloration and the shedding of large sheets of skin. Symptoms include severe pain and itching, heart rate and temperature change, dehydration, and nail deformities. A flareup is considered a medical emergency because the skin damage and inflammation can cause fluid and electrolyte imbalances, hypothermia, fever, severe infections, and even heart failure.
Treating Psoriasis
Treatment of psoriasis is determined by the type and severity of the condition, the symptoms, and the affected parts of the body. In addition to a primary care provider, treatment may involve a dermatologist, rheumatologist, cardiologist, gastroenterologist, physical and occupational therapists, and a mental health specialist. Treatment modalities may include:
- Topicals, including topical steroids to reduce itching and inflammation, over the counter cortisone ointment, vitamin D creams to reduce the rate at which skin cells grow, coal tar, which reduces inflammation and scaling, topical retinoids to help reduce inflammation, and moisturizers to soothe dry skin.
- Phototherapy, which involves exposing the skin to UVA and UVB rays
- Systemic treatments, including oral, injectable or intravenous biologic and biosimilar medications
- Immunosuppressives, such as methotrexate or cyclosporine, to help calm the overactive immune system
Reducing Flare-Ups
If you suffer from psoriasis, it’s especially important to maintain a healthy lifestyle:
- Eat a healthy diet. Avoid red meat, processed foods, sugar, and refined carbs. Instead, choose healthy, anti-inflammatory foods like fruits, veggies, whole grains, nuts, seeds, and fatty fish.
- Exercise regularly. It helps you maintain a healthy weight and help reduce inflammation. Manage stress. Yoga, meditation, deep breathing, and cognitive-behavioral therapy can help. Quit smoking. Nicotine is a known trigger.
- Limit alcohol. It can trigger flare-ups and interact with medications.
- Moisturize regularly. Keep skin moist to reduce scaling and drink plenty of water to stay hydrated.
- Use sunscreen. While a moderate amount of sun may be helpful, sunburn can trigger flare-ups.
- Stick to your medical treatment.
The Koebner Phenomenon
People with psoriasis and certain other skin diseases are susceptible to the Koebner phenomenon, in which an injury to the skin can trigger new lesions. The Koebner phenomenon can arise after an injury that penetrates both the top layer (epidermis) and middle layer (dermis) of the skin, including injections, piercings, puncture wounds, bug bites, tattoos, tattoo removals, and burns. This is more likely to happen if you are already experiencing a flareup. Koebner-related lesions appear 1-20 days after an injury and run in a straight line. If you have been diagnosed with psoriasis or other skin diseases, exercise caution to prevent injuries and talk to your doctor before getting a new tattoo or piercing.
If you have a skin condition that doesn’t clear up, or have experience changes in your skin recently, it’s important to talk to your doctor to get a diagnosis and appropriate treatment. Find a doctor who’s right for your needs.
This article first appeared in the August 2025 edition of the HealthPerks newsletter.

